On 21 July 2021, the Care Quality Commission (CQC) published data showing death notifications involving COVID-19 received from individual care homes between 10 April 2020 and 31 March 2021.
Transparency is an essential component of care delivery, and this report fulfils the CQC’s commitment to publish data at this level. The information contained in the report acts as a reminder of the severe impact the COVID-19 pandemic has had on elderly care home residents, their families, and those who cared for them. It is therefore tremendously sensitive.
As analysts to the elderly care home sector, while remaining sensitive to the pain and suffering that lies behind these numbers, we’ve looked deeper into this data to see if there are any trends or patterns that emerge. We have not performed this analysis at individual care home level. Instead, we have looked at it in the aggregate, assessing whether there is a correlation between death notifications involving COVID-19 across England and factors such as en-suite provision, wetroom provision, size of home, and CQC rating.
Key findings
One of the most notable datapoints to emerge from this release is that 31% of elderly care homes had zero deaths involving COVID-19 during the time period in question. The virus has taken a terrible toll on many thousands of elderly care home residents, their families, and the staff who cared for them, but it is also now clear that a significant proportion of elderly care homes successfully navigated the pandemic without suffering a single COVID-19 death. This is in stark contrast to the sensationalist media representation of the sector – in particular during the first wave of the virus – which sweepingly characterised care homes as fundamentally unsafe.
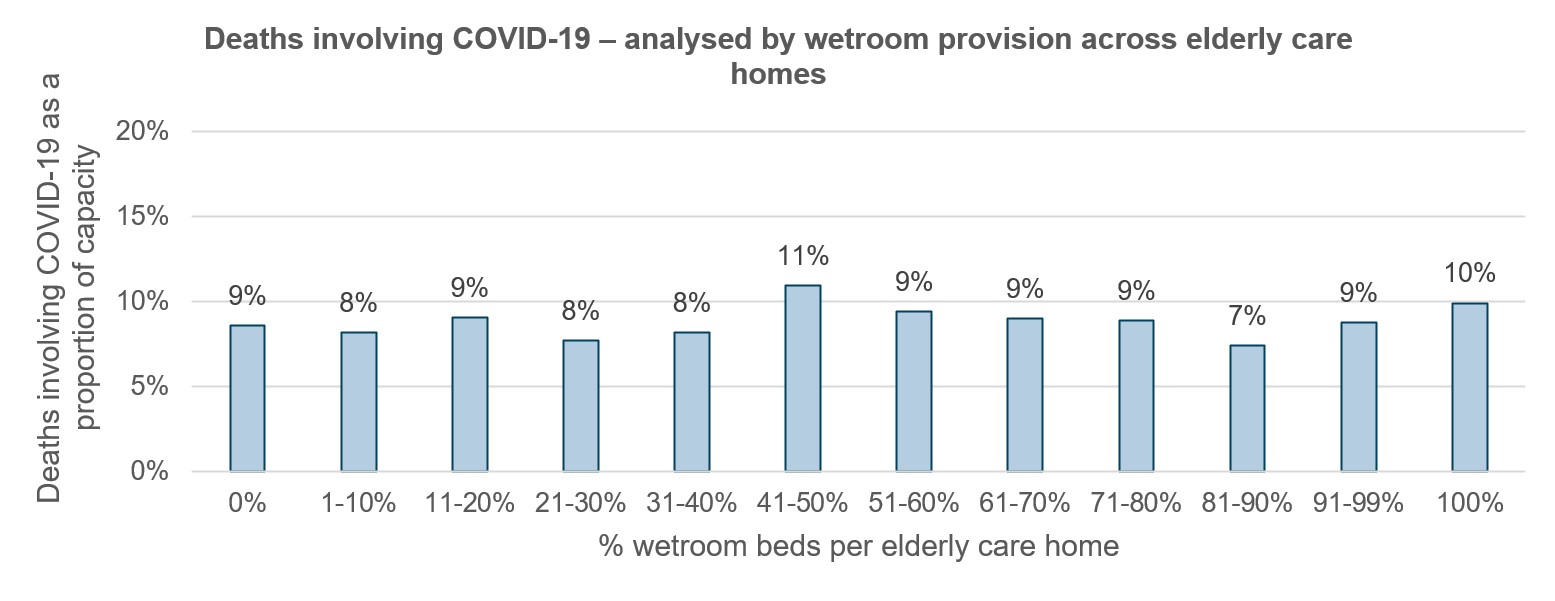
When assessing deaths involving COVID-19 against different care home characteristics, just one of the four assessed here – size – shows a correlation.
Larger homes (41+ total beds) experienced higher rates of deaths involving COVID-19 (relative to their total capacity) than smaller homes. We would expect this, given that a higher number of residents necessitates a higher number of staff, as well as generating a higher number of visitors to that care home. Intuitively, it makes sense that this higher concentration of people would make it easier for transmission to occur from the wider community into the home, as well as between residents internally. Larger homes also lean towards a nursing care registration, which in broad terms means a frailer, more vulnerable resident population with lower resilience to the effects of the COVID-19 virus.
That aside, it appears that the incidence of COVID-19, even within larger homes, was largely indiscriminate when it comes to the type of elderly care home it affected, instead likely being driven primarily by the severity of the infection in the local community each home was situated within.
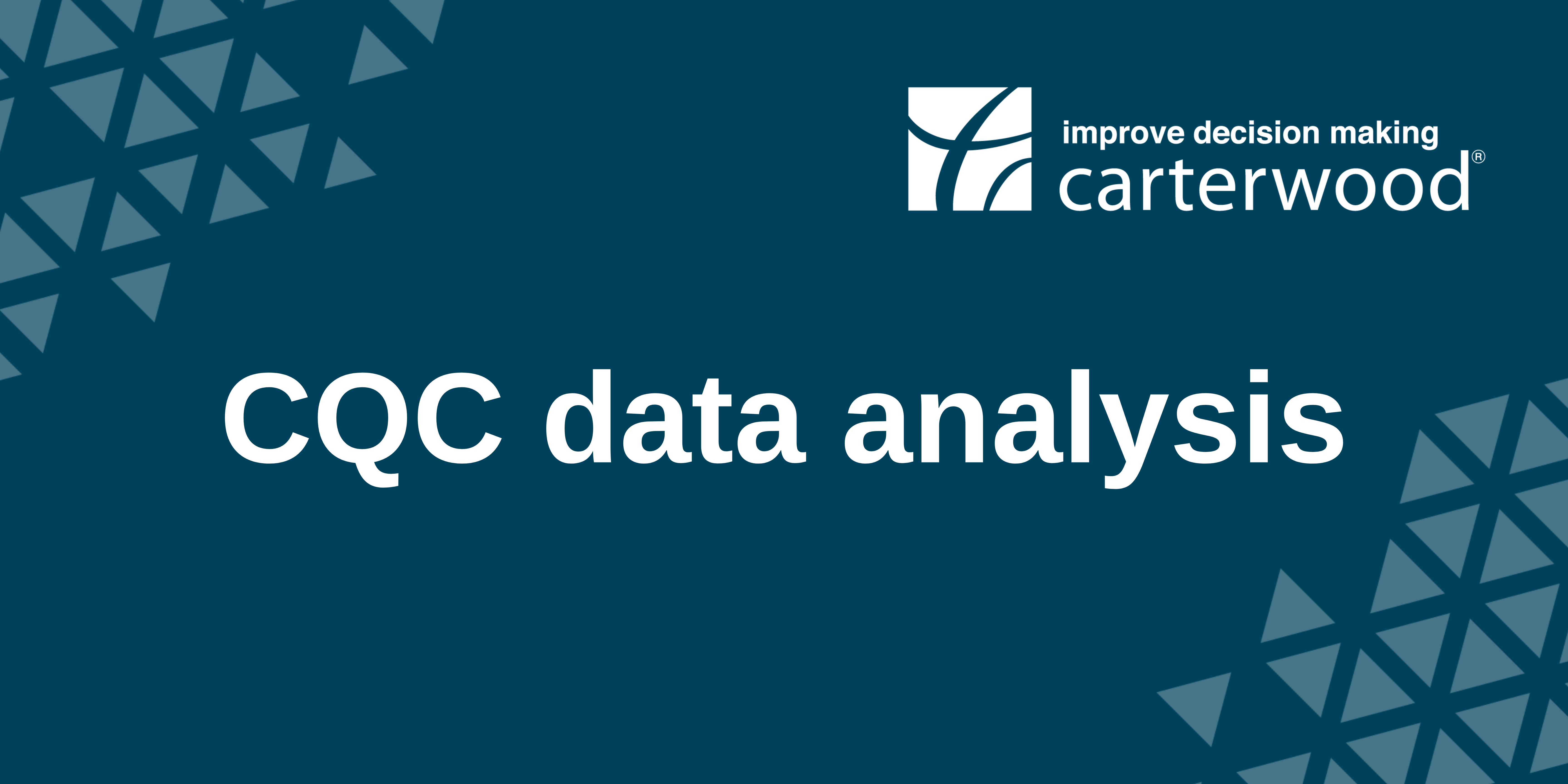
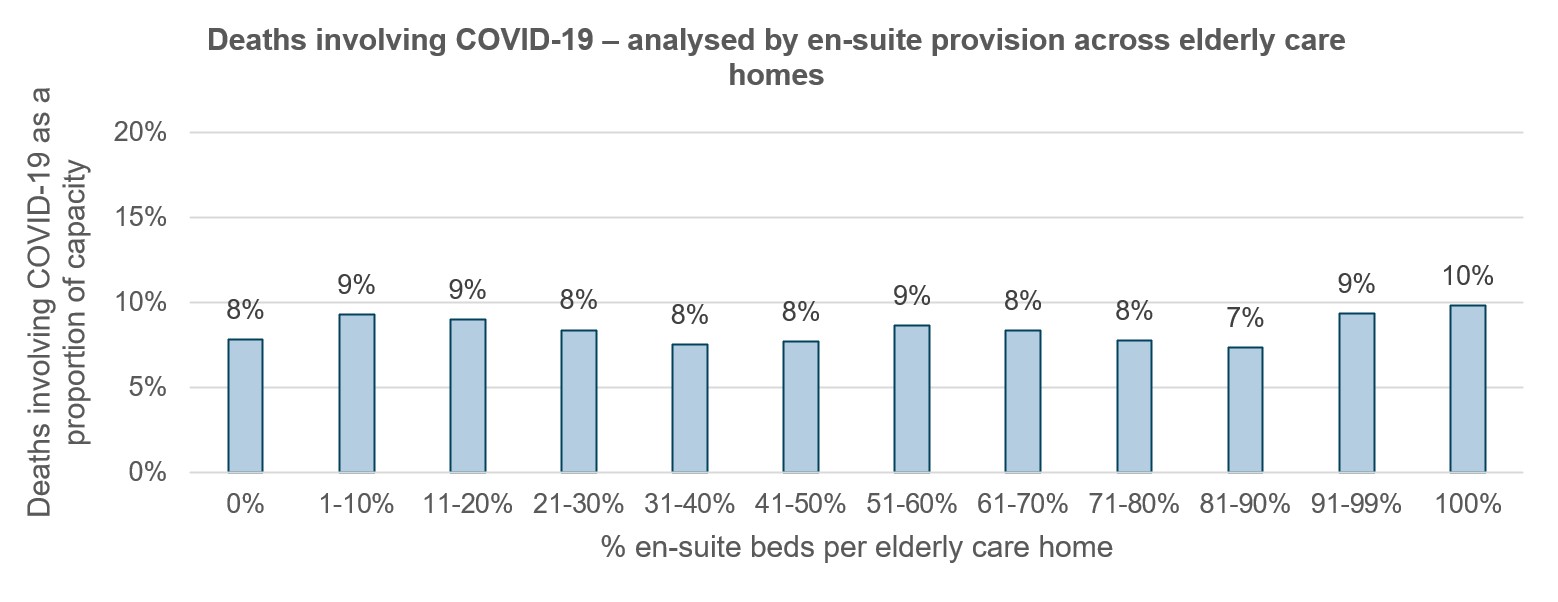
We observe no correlation between levels of en-suite provision, wetroom provision, or CQC rating, and deaths involving COVID-19.
It is also important to be mindful of some caveats the CQC included in their release:
- ‘Although this data relates to deaths of people who were care home residents, many of them did not die in or contract COVID-19 in a care home’ (Source).
- ‘For example, a resident may have been admitted from a care home to hospital with a fracture, contracted COVID-19 while in hospital, and subsequently died without returning to the care home’ (Source).
The CQC’s data suggests that within the published dataset, 25% of elderly care home resident deaths involving COVID-19 occurred in hospital.
The data
Observations:
- No correlation between provision of en-suite accommodation and elderly care home deaths involving COVID-19
Observations:
- No correlation between provision of wetroom accommodation and elderly care home deaths involving COVID-19
Observations:
- Smaller elderly care homes (<=40 total beds) experienced fewer deaths involving COVID-19 as a proportion of their total capacity.
- This is likely the result of larger homes having a higher concentration of people (residents, staff, visitors), meaning there was a greater chance of infection from the wider community.
- Larger homes also lean towards a nursing care registration, which in broad terms means a frailer, more vulnerable resident population with lower resilience to the effects of the COVID-19 virus.
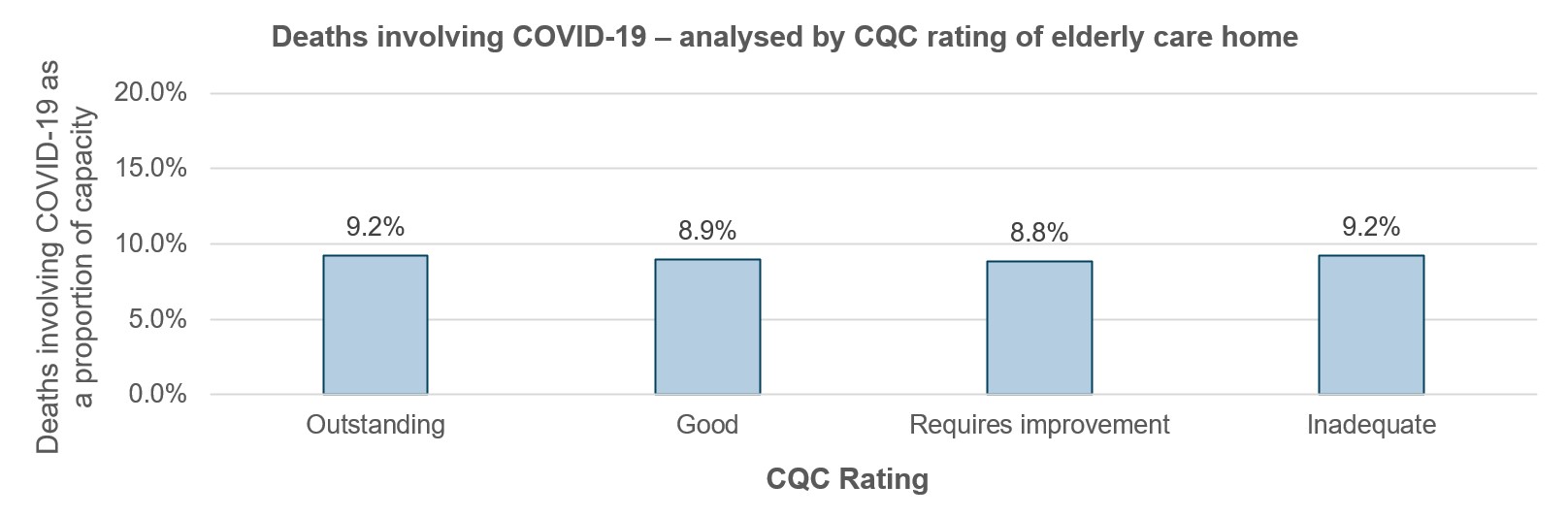
Observations:
- No correlation between provision of CQC rating and elderly care home deaths involving COVID-19
Notes
- Capacity based on total registered beds. We are not able to make any provision for occupancy, given the lack of available data
- Assumes any home not in CQC list has had zero deaths during the time period in question
- Only includes elderly homes that were operational at the time of research
Sources
- Care Quality Commission, Tomorrow’s Guide, Carterwood
For more information, please contact Dan Madden – head of marketing – on dan.madden@carterwood.co.uk.